By: Joshua F. Robinson*, Ioatzin Rios de Anda, Fergus J. Moore, Florence K. A. Gregson, Jonathan P. Reid, Lewis Husain, Richard P. Sear & C. Patrick Royall
 One of the major strategies in response to the spread of the SARS-CoV-2 virus that transmit the COVID-19 disease is effective utilization of personal protective equipment (PPE). Among the list of PPEs, different kinds of face masks have been highly recommended especially for activities in indoor spaces, public transports and some public places. Recommendations for PPEs and the use of different variants of face coverings at different places for mitigations and preventing virus transmission remain a topic of debate as to their effectiveness in preventing the spread of the virus.
One of the major strategies in response to the spread of the SARS-CoV-2 virus that transmit the COVID-19 disease is effective utilization of personal protective equipment (PPE). Among the list of PPEs, different kinds of face masks have been highly recommended especially for activities in indoor spaces, public transports and some public places. Recommendations for PPEs and the use of different variants of face coverings at different places for mitigations and preventing virus transmission remain a topic of debate as to their effectiveness in preventing the spread of the virus.
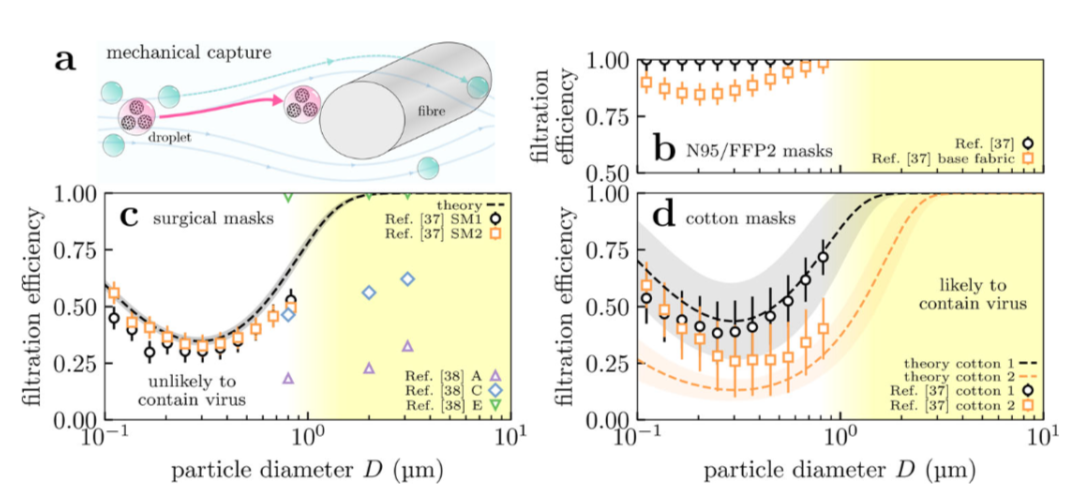
Josh F. Robinson et.al from the University of Bristol, UK have developed a model that predicts the effectiveness and filtration efficiencies of various types of face mask in terms of the mask materials and structures. The proposed model combines a given mask’s material filtration and leakage with three biological factors including; the distribution of respired aerosol particles, the viral load of the exhaler as well as the probability of deposition in the respiratory tract of the inhaler. They found that, indeed, masks do protect the wearer, but perform best as source control; in any case, masking both the exhaler and inhaler is best. But with caution as noted by the authors, not all masks are the same. Surgical masks are effective at reducing the risk of airborne transmission because the filtering material used in most surgical masks are highly effective at filtering respirable particles with diameters ≥1μm. Surgical masks are however, significantly less effective mostly due to the poor fit compared to masks, such as FFP2 (filtering facepiece) and N95.
This issue’s Newsletter Committee:
Editor | Kerry Kelly, University of UtahSenior Assistant Editor | Krystal Pollitt, Yale UniversityJunior Assistant Editor | Justice Archer, University of BristolGuest Contributor | Dong Gao